Heart failure with preserved ejection fraction (HFpEF) is increasingly recognized as a common subtype of heart failure, particularly in older adults and women over the age of 65. Despite representing more than half of heart failure cases in this demographic, HFpEF is still underdiagnosed in primary care. A major reason lies in the limitations of diagnostic tools such as N-terminal pro B-type natriuretic peptide (NT-proBNP). This highlights the critical role of NT-proBNP testing in HFpEF and why its limitations must be addressed.
NT-proBNP Testing in HFpEF: Why Diagnosis is Difficult
NT-proBNP is secreted in response to myocardial wall stress and is an established biomarker in heart failure. Its diagnostic sensitivity and specificity, however, vary depending on the type of heart failure:
- Heart Failure with Reduced Ejection Fraction (HFrEF): NT-proBNP levels are typically elevated, making it highly reliable.
- HFpEF: Levels are often lower, creating a risk of false negatives.
Other influencing factors include:
- Age: Elderly patients naturally present with higher baseline NT-proBNP.
- Renal function: Impaired clearance inflates NT-proBNP values.
- Obesity: Can suppress NT-proBNP levels, masking HFpEF and leading to false reassurance.
This complexity reduces the biomarker’s reliability in detecting HFpEF in older patients—particularly women with multiple comorbidities—where interpretation must always be contextualized. Therefore, NT-proBNP testing in HFpEF should never be interpreted in isolation but always in the full clinical context.
Missed Diagnoses in Primary Care
Women over 65 remain the most vulnerable group for delayed HFpEF diagnosis. Many present with symptoms consistent with heart failure, yet their NT-proBNP levels may not reach diagnostic thresholds. As a result, cases often remain undetected until acute decompensation occurs, leading to emergency admissions.
In the UK, research shows that only 17–22% of patients with suspected HF undergo NT-proBNP testing prior to referral to secondary care, highlighting underuse and inconsistency. This represents a missed opportunity for earlier intervention.
This underlines how NT-proBNP testing in HFpEF must be prioritized to prevent missed diagnoses in high-risk patients.
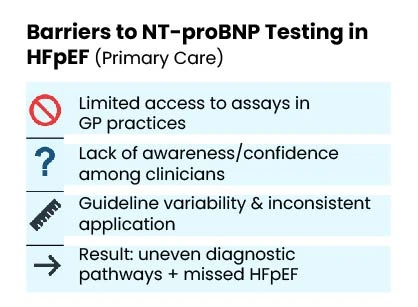
Why Testing Rates Remain Low
Barriers to wider NT-proBNP adoption in primary care include:
- Limited access to assays in GP practices.
- Knowledge gaps among clinicians or lack of confidence in interpreting results.
- Guideline variability, leading to inconsistent application.
As a result, many GPs bypass NT-proBNP and rely instead on ECG or direct referral to echocardiography—approaches that create uneven diagnostic pathways and increase the likelihood of missed HFpEF. Improving access to NT-proBNP testing in HFpEF is essential to strengthen consistency across primary care pathways.
Clinical Implications of Delayed or Missed HFpEF Diagnoses
The consequences of underusing NT-proBNP in HFpEF are significant:
- Treatment delays that allow disease progression.
- Higher emergency hospital admission rates due to late detection.
- Worsened outcomes and mortality, particularly in older women.
Overreliance on NT-proBNP as a standalone test also risks overlooking other critical diagnostic clues, such as diastolic dysfunction, left atrial pressure, or coexisting conditions like atrial fibrillation, diabetes, and chronic kidney disease. By expanding NT-proBNP testing in HFpEF and combining it with complementary tools, many of these risks can be mitigated.
Pathway to Better Outcomes
Improved outcomes require:
- Raising awareness among primary care providers about NT-proBNP limitations.
- Expanding access to testing in general practice.
- Integrating complementary tools such as echocardiography-equivalent device-based diagnostics (e.g., Cardio-HART) to strengthen the diagnostic pathway.
- Contextual interpretation of NT-proBNP results, never using it in isolation.
Such measures can help prevent missed diagnoses, support timely treatment initiation, and reduce hospital admissions. Improving NT-proBNP testing in HFpEF is a key step toward earlier detection and better patient outcomes.
Key Takeaways
- NT-proBNP remains valuable in heart failure diagnosis but shows limited sensitivity in HFpEF, especially in older women.
- Testing remains underutilized in UK primary care, with only 17–22% of suspected HF patients tested before referral.
- Reliance on NT-proBNP alone risks false negatives in obese patients and false reassurance in elderly populations.
- Broader access to testing, better education, and integration of advanced diagnostics are needed for timely and accurate HFpEF detection.
Related reading
NT-proBNP and Diabetes: Risks of Misdiagnosis in Heart Failure
NT-proBNP in Heart Failure Diagnosis: Challenges, Clinical Effectiveness, and the Need for More Accurate Tools
NT-proBNP in Heart Failure Diagnosis: Clinical Delay, Biomarker Limits, and the Need for Diagnostic Reinvention
The Impact of Obesity on NT-proBNP in Heart Failure: Focus on HFpEF and Early Diagnosis
References & Data Sources
1. McMurray, J. J. V., et al. (2021). “NT-proBNP Testing in the Diagnosis of Heart Failure: Is It Enough?” Journal of the American College of Cardiology, 77(7), 837–846.
2. National Institute for Health and Care Excellence (NICE). (2018). Chronic Heart Failure in Adults: Diagnosis and Management. NICE guideline NG106.
3. Doering, G., et al. (2020). “Electrocardiographic Biomarkers in Heart Failure Diagnosis.” Circulation, 142(18), 1732-1745.
4. Cleland, J. G. F., et al. (2019). “The Role of NT-proBNP in Heart Failure Diagnosis.” European Heart Journal, 40(21), 1717-1723.