LVEF in Primary Care is becoming essential as heart failure (HF) continues to rise globally, driven by population ageing and the increasing prevalence of hypertension, diabetes, and obesity. In the UK, around 900,000 people live with heart failure, and projections suggest this number will rise by 25% over the next two decades. Early detection matters: delayed diagnosis leads to disease progression, avoidable hospital admissions, and worse outcomes.
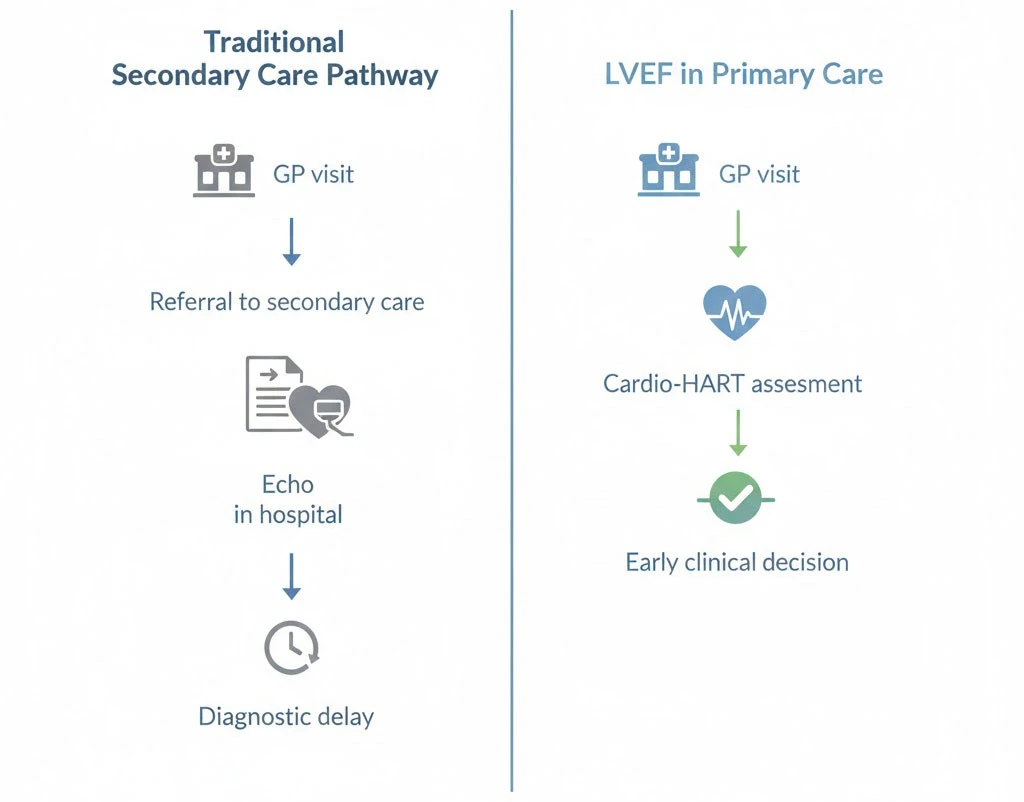
In most healthcare systems, accurate HF diagnosis still depends on echocardiography, which is commonly accessed through secondary care. This creates delays, especially when patients first present in general practice with non-specific symptoms such as shortness of breath, fatigue, or fluid retention. A key reason for delayed diagnosis is limited access to functional cardiac assessment—particularly Left Ventricular Ejection Fraction (LVEF)—at the point of care.
Why LVEF in Primary Care Matters for Heart Failure Diagnosis
LVEF is the percentage of blood pumped out of the left ventricle with each heartbeat. It is a central marker of cardiac performance and one of the most important measures used to classify heart failure. In healthy individuals, LVEF typically ranges from 55% to 70%. When LVEF falls below 40%, it usually indicates significant systolic dysfunction and is strongly associated with Heart Failure with Reduced Ejection Fraction (HFrEF).
LVEF is also critical for distinguishing between HF phenotypes:
- HFrEF: typically LVEF <40%, reflecting impaired contractility
- HFpEF: LVEF often normal or near-normal, but the heart has impaired relaxation and filling, causing HF symptoms despite preserved ejection function
This distinction is not academic—it influences treatment pathways, prognosis, and referral urgency. HFpEF is especially difficult to detect early because LVEF may appear “normal,” and symptoms can overlap with non-cardiac causes.
The Diagnostic Gap in Primary Care
Echocardiography remains the reference standard for LVEF measurement, but it requires specialised equipment and trained staff. This often places LVEF assessment outside the reach of primary care, forcing clinicians to rely on symptoms, physical examination, and ECG—tools that may not reliably detect early structural or functional dysfunction.
The consequences are predictable:
- delayed diagnosis and late treatment initiation
- high referral volume to echocardiography services
- bottlenecks and long waiting times
- missed early-stage disease, particularly HFpEF
In practice, primary care often becomes a “waiting room” for confirmation testing rather than an active diagnostic hub.
Bringing LVEF in Primary Care Into Everyday General Practice
Integrating LVEF assessment into primary care represents a major shift in how early HF can be identified. When GPs can assess LVEF at the point of care, the initial consultation becomes far more clinically actionable. Early functional assessment helps determine whether symptoms are likely cardiac in origin and supports quicker decision-making about referral urgency.
Modern point-of-care diagnostics can support LVEF measurement alongside additional parameters often associated with echocardiography, such as:
- structural and functional markers of cardiac dysfunction
- signs of diastolic impairment relevant to HFpEF
- indicators of myocardial abnormalities
- assessment of valve function contributing to HF symptoms
This allows a more complete cardiovascular assessment during the first presentation, rather than weeks later.
Cardio-HART as a Point-of-Care Diagnostic Approach
Cardio-HART combines ECG with echocardiography-like diagnostic capabilities, including LVEF assessment and broader functional insights. Its value in primary care is not simply in producing an LVEF number, but in enabling a more comprehensive evaluation of cardiac function in a quick, non-invasive test.
By expanding what can be assessed in general practice, Cardio-HART can support earlier recognition of heart failure—particularly cases that are commonly missed with ECG alone. In published evidence, Cardio-HART in primary care settings improved early detection of heart failure compared to traditional ECG-based approaches. Earlier detection enables earlier intervention, which is strongly associated with fewer admissions and improved outcomes.
Cardio-HART’s broader assessment may be particularly helpful in HFpEF, where diagnosis often depends on identifying subtle dysfunction that may not be obvious through symptoms or ECG, and may not be detected early enough in delayed echo pathways.
NT-proBNP as a Complementary Biomarker in Primary Care
NT-proBNP is a biomarker released when the heart is under stress. Elevated levels can support heart failure suspicion and help differentiate cardiac from non-cardiac causes of symptoms like dyspnoea. NT-proBNP is clinically useful, but it does not directly measure heart function or define HF phenotype.
This is where combining NT-proBNP with LVEF becomes valuable:
- NT-proBNP helps indicate cardiac stress and supports triage
- LVEF provides functional confirmation and helps classify HF subtype
- together they improve diagnostic accuracy and decision confidence
Evidence suggests that combining NT-proBNP with LVEF improves diagnostic sensitivity, especially in HFpEF where NT-proBNP alone may be less definitive. This approach also supports ongoing monitoring: serial NT-proBNP levels alongside LVEF trends can help evaluate treatment response and disease progression.
Making Primary Care the Centre of Early Heart Failure Diagnosis
When LVEF assessment and NT-proBNP testing are integrated into primary care, the diagnostic pathway shifts from delayed confirmation to earlier action. This can reduce reliance on overloaded secondary-care imaging pathways and allow hospitals to focus on more complex cases.
The system impact is substantial. Earlier diagnostics in primary care can reduce referrals, improve prioritisation, and lower overall costs. Evidence suggests early diagnostic strategies can reduce total HF management costs by up to 30%. More importantly, earlier diagnosis is linked to improved survival, particularly when disease is identified before severe symptoms develop.
Beyond system efficiency, patient experience improves when diagnosis and early management happen closer to home. Earlier clarity also supports better adherence to treatment and stronger continuity of care.
Summary
LVEF is a cornerstone measurement in heart failure diagnosis, classification, and treatment planning, yet it has historically been inaccessible in primary care because it required echocardiography in secondary care settings. Integrating LVEF assessment into general practice, supported by point-of-care diagnostic tools like Cardio-HART and complemented by NT-proBNP testing, enables earlier and more accurate diagnosis—especially for HFpEF. This shift can accelerate treatment decisions, reduce unnecessary referrals, relieve pressure on echocardiography services, and improve outcomes for patients.
Related reading
NT-proBNP and Diabetes: Risks of Misdiagnosis in Heart Failure
NT-proBNP in Heart Failure Diagnosis: Challenges, Clinical Effectiveness, and the Need for More Accurate Tools
NT-proBNP in Heart Failure Diagnosis: Clinical Delay, Biomarker Limits, and the Need for Diagnostic Reinvention
The Impact of Obesity on NT-proBNP in Heart Failure: Focus on HFpEF and Early Diagnosis
NT-proBNP Testing in Heart Failure with Preserved Ejection Fraction (HFpEF): Diagnostic Challenges and Clinical Implications
The Decision to Order NT-proBNP: How ECG Findings and Clinical Factors Influence Testing
Evaluating NT-proBNP Thresholds and Referral Pathways in Heart Failure Diagnosis: A Comparative Analysis of NHS and EU Practices
Device-Based Heart Failure Diagnostics: Why Tools Beyond NT-proBNP Are Needed