Executive Summary
Device-based heart failure diagnostics are increasingly recognized as essential to complement NT-proBNP testing. Although NT-proBNP remains central to current diagnostic pathways, clinical evidence and guideline recommendations highlight clear limitations—particularly in HFpEF and complex patient populations. This article outlines why tools delivering echocardiography-like outputs are needed to improve accuracy, reduce delays, and relieve pressure on healthcare systems.
Introduction: The Diagnostic Challenge of Heart Failure
Heart failure (HF) remains one of the leading causes of morbidity, hospital admissions, and mortality worldwide. Early and accurate diagnosis is essential to improving outcomes, reducing disease progression, and optimizing healthcare resource utilization.
In current clinical practice, NT-proBNP testing is widely used as a frontline biomarker to support heart failure diagnosis and guide referral pathways. However, biomarker-based diagnosis alone has important limitations, particularly in primary care and in patients with complex comorbidities.
Recognizing these challenges, NICE guideline NG106 explicitly calls for further research into diagnostic devices capable of providing findings comparable to echocardiography, signaling a shift toward more integrated and device-based diagnostic strategies.
Limitations of NT-proBNP Testing in Clinical Practice
NT-proBNP is highly valuable as a rule-out test, but its diagnostic performance is influenced by multiple non-cardiac factors, including:
- Advanced age
- Chronic kidney disease
- Obesity
- Atrial fibrillation
- Diabetes and metabolic disorders
These confounders can result in:
- False-positive results, leading to unnecessary referrals and investigations
- False-negative results, particularly in early or atypical presentations
As a result, NT-proBNP alone cannot reliably distinguish heart failure from other causes of symptoms such as dyspnea or fatigue.
HFpEF: Where NT-proBNP Performs Least Reliably
Heart Failure with Preserved Ejection Fraction (HFpEF) represents a growing proportion of heart failure cases, especially among:
- Older adults
- Women
- Patients with obesity, hypertension, or diabetes
HFpEF presents a particular diagnostic challenge because:
- NT-proBNP levels are often lower than in HFrEF
- Structural and diastolic abnormalities may be present despite “normal” biomarker values
- Standard ECG lacks sensitivity for functional abnormalities
NICE guidelines acknowledge these diagnostic gaps and emphasize the need for alternative approaches that move beyond biomarkers alone.
System-Level Constraints: Echocardiography Access and Delays
Echocardiography remains the gold standard for confirming heart failure and assessing cardiac structure and function. However, in real-world healthcare systems:
- Access to echocardiography is limited
- Waiting times are often prolonged
- Capacity constraints delay diagnosis and treatment
These system-level constraints increase the risk of:
- Disease progression before diagnosis
- Emergency hospital admissions
- Inefficient use of specialist services
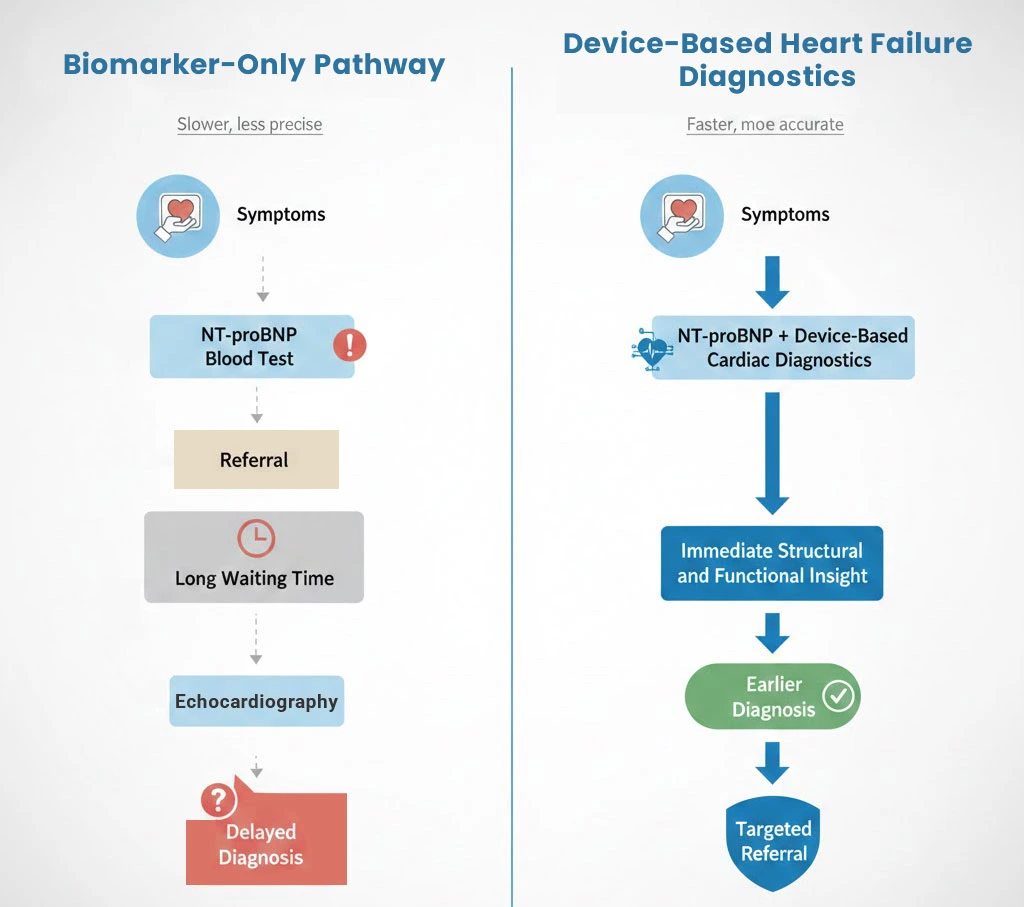
Why Device-Based Heart Failure Diagnostics Are Needed
Device-based heart failure diagnostics enable earlier structural and functional cardiac assessment at the point of care.
Technologies capable of delivering echocardiography-equivalent findings offer a practical solution to current diagnostic limitations.
Key benefits include:
1. Improved Diagnostic Accuracy
By providing direct structural and functional cardiac data, device-based tools can clarify ambiguous NT-proBNP results—especially in HFpEF and borderline cases.
2. Faster Diagnosis and Earlier Intervention
Point-of-care diagnostics reduce the time between symptom presentation and definitive assessment, enabling earlier treatment initiation.
3. Reduced Pressure on Secondary Care
More accurate triage in primary care lowers unnecessary referrals and optimizes specialist resource allocation.
4. Cost-Effectiveness
Earlier and more precise diagnosis reduces downstream costs associated with late-stage heart failure management and avoidable hospital admissions.
Alignment with NICE NG106 and Future Diagnostic Pathways
NICE NG106 explicitly identifies the need for:
“Further research into diagnostic devices capable of providing findings similar to echocardiography.”
This reflects a broader shift toward:
- Context-aware diagnostics
- Integrated clinical decision-making
- Combining biomarkers with device-based cardiac assessment
Rather than replacing NT-proBNP, these tools complement and contextualize biomarker testing, ensuring that results are interpreted against real cardiac function.
Clinical and Healthcare Impact
Device-based heart failure diagnostics have the potential to significantly improve diagnostic accuracy and care pathways across healthcare systems by addressing several critical challenges:
- Reduce misdiagnosis and missed HFpEF cases
- Shorten diagnostic pathways
- Improve patient outcomes
- Increase system efficiency
- Support evidence-based guideline implementation
Conclusion
NT-proBNP remains a valuable component of heart failure diagnosis—but it is not sufficient as a standalone diagnostic strategy.
Clinical evidence and NICE guidance clearly indicate that the future of heart failure diagnosis lies in combining biomarker testing with accessible, device-based diagnostic tools that provide echocardiography-like insights.
Such an integrated approach enables earlier diagnosis, better clinical decisions, reduced healthcare strain, and ultimately improved patient care—particularly in primary care settings where timely diagnosis matters most.
Device-based heart failure diagnostics provide the structural and functional insight needed to overcome the limitations of biomarker-only pathways.
Device-based diagnostic approaches described in this article are reflected in emerging technologies such as Cardio-HART.
Related reading
NT-proBNP and Diabetes: Risks of Misdiagnosis in Heart Failure
NT-proBNP in Heart Failure Diagnosis: Challenges, Clinical Effectiveness, and the Need for More Accurate Tools
NT-proBNP in Heart Failure Diagnosis: Clinical Delay, Biomarker Limits, and the Need for Diagnostic Reinvention
The Impact of Obesity on NT-proBNP in Heart Failure: Focus on HFpEF and Early Diagnosis
NT-proBNP Testing in Heart Failure with Preserved Ejection Fraction (HFpEF): Diagnostic Challenges and Clinical Implications
The Decision to Order NT-proBNP: How ECG Findings and Clinical Factors Influence Testing
Evaluating NT-proBNP Thresholds and Referral Pathways in Heart Failure Diagnosis: A Comparative Analysis of NHS and EU Practices