NT-proBNP in HFpEF diagnosis is increasingly recognized as a challenge, particularly among older women. Addressing these diagnostic challenges is critical because HFpEF now represents more than half of all heart failure cases in older adults, and timely recognition can substantially reduce hospital admissions. Despite its growing significance, HFpEF remains frequently underdiagnosed in primary care due to the limitations of diagnostic tools such as NT-proBNP. While NT-proBNP is widely used, especially in emergency settings, its role in detecting HFpEF is more complex and often less reliable.
NT-proBNP and HFpEF
Understanding the limits of NT-proBNP in HFpEF diagnosis is critical for avoiding false negatives and improving patient outcomes. NT-proBNP is secreted in response to myocardial stress and is a cornerstone biomarker for heart failure diagnosis. However, its sensitivity and specificity in HFpEF are variable. Compared to heart failure with reduced ejection fraction (HFrEF), NT-proBNP levels in HFpEF tend to be lower, resulting in potential false negatives.
Moreover, NT-proBNP levels are influenced by:
- Age – baseline elevation in elderly patients.
- Renal function – impaired clearance inflates NT-proBNP values.
- Obesity – may suppress NT-proBNP, leading to underdiagnosis.
This complexity reduces NT-proBNP’s reliability in identifying HFpEF, particularly in older adults with multiple comorbidities.
Clinicians must therefore interpret NT-proBNP results in the context of the patient’s overall risk profile, rather than relying on the biomarker alone. Combining NT-proBNP with imaging or advanced diagnostic tools can improve detection and prevent missed cases.
Missed Diagnoses in Primary Care
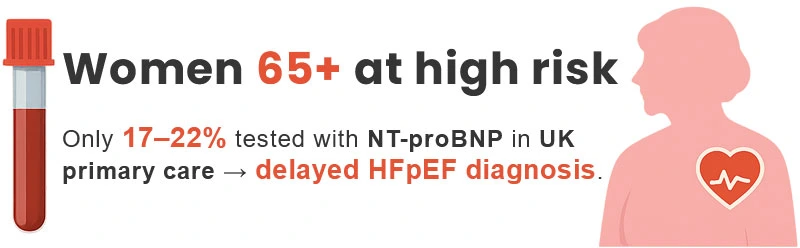
Women over 65 are at particularly high risk for HFpEF, yet many present with NT-proBNP levels insufficient to trigger further evaluation. As a result, diagnoses are often delayed until acute decompensation requires emergency admission. In the UK, studies show that prior to referral to secondary care, only 17–22% of patients suspected of HF undergo NT-proBNP testing, highlighting both underuse and missed opportunities for earlier detection. This gap highlights the importance of strengthening primary care pathways, ensuring that NT-proBNP testing is both accessible and consistently applied when HFpEF is suspected. The low use of NT-proBNP in HFpEF diagnosis is one of the reasons older women often face delayed detection.
Factors Limiting NT-proBNP Testing Rates
Low testing rates are influenced by:
- Limited access to NT-proBNP assays in general practice.
- Lack of awareness or confidence among clinicians.
- Variability in guideline implementation.
Consequently, NT-proBNP is often bypassed in favour of ECG or direct referral to echocardiography, creating inconsistencies in practice.
Clinical Implications
Missed or delayed HFpEF diagnoses carry significant consequences:
- Delays in treatment initiation.
- Increased emergency hospital admissions.
- Worsened outcomes and higher mortality.
Overreliance on NT-proBNP as a standalone tool may also obscure other critical diagnostic elements such as diastolic dysfunction, left atrial pressure, and comorbidities like atrial fibrillation, diabetes, or chronic kidney disease. Relying solely on NT-proBNP in HFpEF diagnosis risks missed cases and worsened outcomes.
Improving education for healthcare providers, expanding access to testing, and integrating complementary diagnostics such as device-based assessments are all steps that could mitigate these risks and improve long-term outcomes.
Key Takeaways
NT-proBNP testing remains valuable in the diagnostic pathway for heart failure but has notable limitations in HFpEF—especially in older women. Its underuse in primary care, combined with interpretive challenges, contributes to late diagnoses and poorer outcomes. Improved awareness, broader access to testing, and integration of additional diagnostic tools beyond NT-proBNP are essential to ensure timely and accurate identification of HFpEF.
Related reading
NT-proBNP and Diabetes: Risks of Misdiagnosis in Heart Failure
NT-proBNP in Heart Failure Diagnosis: Challenges, Clinical Effectiveness, and the Need for More Accurate Tools
NT-proBNP in Heart Failure Diagnosis: Clinical Delay, Biomarker Limits, and the Need for Diagnostic Reinvention
The Impact of Obesity on NT-proBNP in Heart Failure: Focus on HFpEF and Early Diagnosis
References & Data Sources
1. Cleland JGF, et al. European Cardiovascular Disease. 2007;3(1):41–42.
2. Birrel L, et al. British Journal of Cardiology. 2024.
3. National Institute for Health and Care Excellence (NICE). Chronic Heart Failure in Adults: Diagnosis and Management. NG106, 2018.
4. McMurray JJV, et al. European Heart Journal. 2020;41(23):2413–2420.
5. Horwich TB, et al. J Am Coll Cardiol. 2021;77(9):1210–1217.