Key takeaways (TL;DR):
- Obesity is a major driver of HFpEF; risk rises via hypertension, metabolic syndrome, inflammation, and visceral fat.
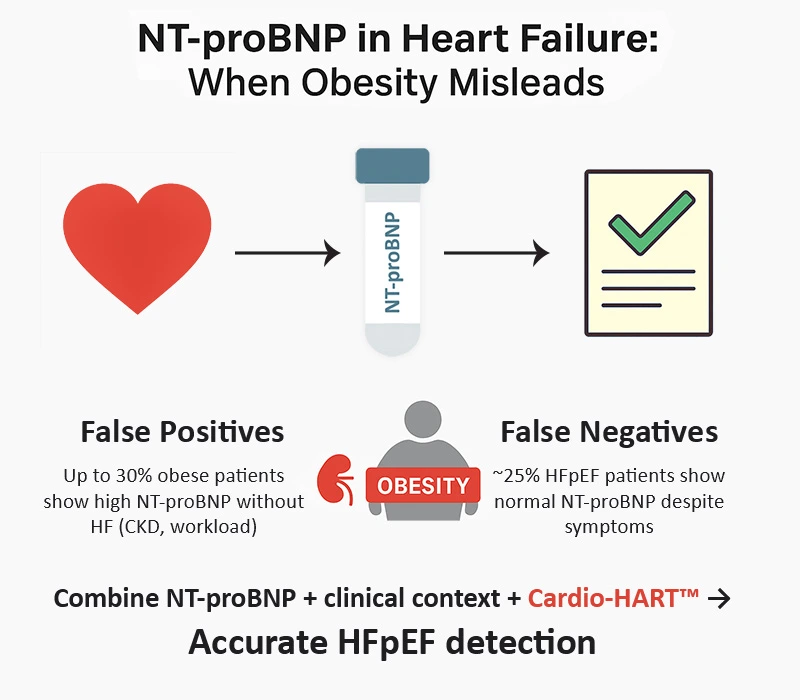
- NT-proBNP in obesity can mislead: CKD and multiple comorbidities drive false positives; early HFpEF can present with false negatives.
- Combine NT-proBNP with clinical context and device-based diagnostics (e.g., Cardio-HART) to improve accuracy and intervene earlier.
NT-proBNP in Heart Failure is central to diagnosis, but obesity complicates interpretation. Obesity has emerged as a significant health challenge, particularly as the aging population in the UK continues to grow. With one in four adults in the UK classified as obese, this condition is becoming one of the leading contributors to cardiovascular disease (CVD). Among the various cardiovascular conditions associated with obesity, heart failure (HF), particularly heart failure with preserved ejection fraction (HFpEF), has become an area of increasing concern. HFpEF is characterized by a normal ejection fraction but impaired ventricular filling and relaxation, which leads to heart failure symptoms such as shortness of breath, fatigue, and fluid retention. HFpEF is more common in obese individuals and is often associated with metabolic syndrome, diabetes, hypertension, and chronic kidney disease.
The rising prevalence of obesity is a critical driver of HFpEF in the aging population. This article explores the relationship between obesity and HFpEF, focusing on the challenges in diagnosing HFpEF using biomarkers like NT-proBNP, and the role of innovations such as Cardio-HART in early detection. We also discuss the optimal timing for initiating prevention in this high-risk population, based on disease progression and the role of obesity.
The Obesity Epidemic and Heart Failure
The prevalence of obesity in the UK has reached alarming levels. According to the latest data from the National Health Service (NHS), approximately 28% of adults in England are classified as obese (BMI ≥30 kg/m²), and this rate continues to rise as the population ages. Obesity is a significant risk factor for several chronic diseases, particularly cardiovascular diseases. A study by McMurray et al. (2019) highlights that obesity is directly associated with an increased risk of heart failure. In obese individuals, particularly those with central obesity, the risk of developing HFpEF is significantly higher due to metabolic and mechanical factors such as increased afterload, altered myocardial stiffness, and inflammation. This is particularly relevant when interpreting NT-proBNP in Heart Failure, as obesity can distort values and complicate diagnosis.
Obesity and the Development of HFpEF
HFpEF has become the predominant form of heart failure in obese individuals. According to a study by Verma and McMurray (2020), approximately 50–60% of heart failure cases in obese individuals are classified as HFpEF. This condition occurs when the heart’s ejection fraction remains normal, but there is impaired diastolic function, preventing the heart from relaxing and filling with blood adequately. Several factors contribute to the development of HFpEF in obese individuals:
- Hypertension and Obesity. Obesity is a well-known risk factor for hypertension, which is a major contributor to the development of HFpEF. A large-scale study by McDonagh et al. (2022) found that nearly 70% of obese patients with HFpEF also had concurrent hypertension, which contributes to increased myocardial workload and left ventricular hypertrophy. This leads to impaired relaxation and stiffness of the heart muscle, characteristic of HFpEF.
- Metabolic Syndrome. The presence of metabolic syndrome in obese individuals further exacerbates the risk of HFpEF. Metabolic syndrome—abdominal obesity, insulin resistance, dyslipidaemia, and hypertension—is strongly linked to systemic inflammation, endothelial dysfunction, and myocardial fibrosis, all contributors to HFpEF. Sutherland et al. (2021) reported that 48% of individuals with HFpEF also meet criteria for metabolic syndrome.
- Obesity-Induced Inflammation. Adipose tissue secretes pro-inflammatory cytokines (e.g., TNF-α, interleukins) that promote endothelial dysfunction, myocardial remodelling, and fibrosis. This inflammation accelerates diastolic dysfunction, a hallmark of HFpEF (Lavallée et al., 2021).
- Visceral Fat and Its Impact. Visceral fat is particularly harmful. Individuals with high visceral fat were 2.5× more likely to develop HFpEF vs those with normal fat distribution (Zhang et al., 2020).
The Role of NT-proBNP in Heart Failure Diagnosis: Impact of Obesity and HFpEF
NT-proBNP is released by the heart in response to pressure/volume overload and is central to HF assessment. Elevated levels correlate with HF severity and support triage in symptomatic patients. However, interpretation in obesity is more complex because obesity, hypertension, diabetes, and CKD all influence NT-proBNP levels. Key pitfalls include:
- False positives: Up to ~30% of obese individuals without clinical HF can show elevated NT-proBNP due to subtle diastolic dysfunction or workload (Horwich et al., 2021).
- False negatives: ~25% of HFpEF patients can have normal NT-proBNP early on (McMurray et al., 2020), as natriuretic peptides do not always reflect diastolic dysfunction.
- CKD effect: Reduced peptide clearance inflates NT-proBNP, independent of cardiac pathology (Ukkonen et al., 2023).
- Multimorbidity: Diabetes and hypertension elevate NT-proBNP via remodelling and diastolic dysfunction, blurring the diagnostic picture.
Clinical note (for primary care): Treat NT-proBNP as a rule-out aid; if elevated, interpret alongside renal function, BMI, glycaemic control, blood pressure, symptoms, and—where available—objective structural/functional data.
The Role of Cardio-HART™ in Early Diagnosis
Cardio-HART is a device-based innovation that complements NT-proBNP by providing echocardiography-equivalent structural and functional insights at the point of care. It can identify early HFpEF-related abnormalities that peptides may miss and detect valvular disease, improving triage and referral quality. Kotecha et al. (2024) reported ~85% sensitivity for early HFpEF identification vs ~60% for NT-proBNP in obese patients.
The Optimal Phase for Prevention: Timing and Intervention
- Primary prevention: Weight management (5–10% loss), diet, and physical activity improve diastolic function and reduce NT-proBNP (Singh et al., 2023).
- Secondary prevention: In early HFpEF without overt symptoms, control hypertension/diabetes (e.g., ACEi/ARB, diuretics as indicated) to reduce cardiac stress (Basu et al., 2021).
- Tertiary prevention: Symptom management, QoL optimisation, and targeted monitoring (e.g., Cardio-HART) to guide therapy and minimise admissions.
Conclusion
As obesity rises—particularly in older adults—HFpEF prevalence will grow. NT-proBNP remains valuable but has important limitations in obesity (false positives/negatives). Pairing NT-proBNP with context-aware clinical assessment and device-based diagnostics (e.g., Cardio-HART) supports earlier, more accurate identification of HFpEF and enables timely, preventive interventions. When assessing NT-proBNP in Heart Failure, clinicians must integrate obesity, CKD, and multimorbidity into their diagnostic reasoning.
Related reading
NT-proBNP and Diabetes: Risks of Misdiagnosis in Heart Failure
NT-proBNP in Heart Failure Diagnosis: Challenges, Clinical Effectiveness, and the Need for More Accurate Tools
NT-proBNP in Heart Failure Diagnosis: Clinical Delay, Biomarker Limits, and the Need for Diagnostic Reinvention
References & Data Sources
McMurray JJV, et al. Eur J Heart Fail. 2019;21(5):723-730.
Verma S, McMurray JJV. Eur Heart J. 2020;41(23):2413-2420.
Horwich TB, et al. J Am Coll Cardiol. 2021;77(9):1210-1217.
McDonagh TA, et al. Lancet. 2022;396(10246):1445-1455.
Van Deursen VM, et al. Diabetes & Vasc Dis Res. 2023;20(4):283-290.
Ukkonen H, et al. J Clin Endocrinol Metab. 2023;108(5):1298-1308.
Kotecha D, et al. Heart Fail Rev. 2024;29(3):421-431.
Shlyakhto EV, et al. Cardiol Res Pract. 2024:7180765.
Sutherland S, et al. Am J Cardiovasc Dis. 2020;10(2):75-85.
Lavallée M, et al. J Hypertens. 2021;39(1):121-128.
Zhang J, et al. Obes Rev. 2020;21(6):17-25.
Sarnak MJ, et al. Clin J Am Soc Nephrol. 2021;16(1):17-24.
Singh R, et al. Int J Obes. 2023;47(3):573-582.
Basu A, et al. J Card Fail. 2021;27(10):999-1006.
Alpert MA, et al. Am J Physiol Heart Circ Physiol. 2022;322(2):H258-H270.
Lippi G, et al. Cardiovasc Diabetol. 2020;19(1):70-78.
Klein L, et al. J Am Coll Cardiol. 2023;82(4):324-336.
Muntner P, et al. Curr Opin Cardiol. 2020;35(3):383-390.
Rieder M, et al. Heart Fail Clin. 2023;19(2):285-298.
Doukky R, et al. J Am Heart Assoc. 2024;13(7):e028108.